Chapter 1:Introduction
1.1. Background of the study
High blood pressure (hypertension) is one of the most common chronic illnesses in the world that make people more prone to cardiovascular disorders, including heart attacks, strokes and kidney failures. It is a significant contributor to premature mortality and disability in both the global population causing huge health-related costs in the global population. In some forms, hypertension is not usually diagnosed and managed especially during the earlier onset, a factor that worsens its dire health effects (Burnier and Egan, 2019). The aim is to curb such complications through early diagnosis and treatment. Thus, the risk factors related to hypertension as well as their characterization and forecast should be necessary in mitigating the extent of the condition on the health indicators of the population.
The available studies reveal that hypertension applies to people of different ages, but the problem is very alarming among the younger adults, especially those below the age of 40 years. In this population, hypertension occurs under two typologies namely primary and secondary with primary hypertension such as primary aldosteronism contributing to a large percentage of the cases (Connelly, Currie and Delles, 2022). Other causes, which are minor ones, but are equally vital in the development of hypertension, include pheochromocytoma (PPGL), a renovascular problem and nephropathy. The recent trend of high blood pressure among the younger generation is threatening especially because young people are asymptomatic in the initial stages of their illnesses when it is hard to realize or treat the condition before the complications develop.
Moreover, the factors which lead to the occurrence of hypertension are a mixture of genetic, environmental, and lifestyle. Some of the major risk factors are lack of physical activity, obesity, smoking, stress, consumption of alcohol and age though obesity and smoking appear to be the greatest leading contributors of the disease (Meinert, Thomopoulos and Kreutz, 2023). Change in lifestyle like an increment in physical activity, cutting down some alcohol content and stress management are crucial in prevention and control of hypertension. These risk factors will further increase by the day as world populace ages making early detection tools and preventive plans necessary.
Health information like age, sex, level of cholesterol and other medical parameters are valuable data presented in Hypertension Risk Prediction Dataset used in this research, and can be used to predict whether hypertension will occur (Ojangba et al., 2023). By defining significant variables as predictors and using machine learning models, healthcare providers will be able to anticipate the progression of hypertension at the initial stage more efficiently and help to prevent the acquisition of long-term health conditions. The implementation of data-driven solutions in clinical practice can potentially revolutionize the current approach to managing hypertension and can provide more effective and efficient responses to different healthcare systems worldwide (Schmidt et al., 2020).
1.2 Research Problem
Hypertension is a life threatening and common ailment, which greatly exposes individuals to heart attacks, strokes and kidney failure. Regrettably, it's not diagnosed in time so that it gets into its later stages and causes serious health issues. The main reason behind this late diagnosis is that hypertension is symptomless during the initial phases which makes it hard to diagnose without regular screening. The consequence of this is that, early intervention is not common and individuals experience long-term health effects (Song et al., 2019). This has enhanced by the absence of holistic tools in the clinical environment to forecast hypertension when it starts especially among the youth.
The existing predictive models do not take into account the interactions between different risk factors, including age, cholesterol level, lifestyle (smoking, stress, physical activity, and diet), and their joint impact on the development of hypertension. Although the impact of individual risk factors is studied, little research has conducted to combine these factors to provide a more comprehensive perspective on predicting hypertension. Moreover, less known about the role of secondary hypertension, which may cause either by conditions as pheochromocytoma or renovascular problems, especially among younger adults. This research gap complicates the early identification and treatment of secondary hypertension because such conditions are commonly not diagnosed (Trimarco et al., 2022).
It is in these gaps that the proposed research aims to fill by examining the Hypertension Risk Prediction Dataset, which contains these variables: age, sex, blood pressure, cholesterol levels, and lifestyle factors. This data will be used to create a predictive model that will determine individuals with a high risk of developing hypertension so that a healthcare professional can then intervene and avert the development of this disease (van Oort et al., 2020).
This study is significant to the topic of studying the primary and secondary causes of hypertension bearing in mind that prevalence of hypertension is rising with the prevalence being more common among younger adults. It will examine the significance of lifestyle variables that are modifiable, such as a diet, exercises, and stress, which is not well regarded in the modern research. The correlation of these variables into a general predictive model will allow this research to improve the early detection and prevention of hypertension that will ultimately help to reduce its health-related impacts and provide feasible guidelines to the medical community (Wen et al., 2019).
Get reliable Assignment Help Edinburgh from subject-matter experts you can trust.
1.3. Research Rationale
Hypertension is among the top causes of death occurrences that are preventable across the world and a significant cause of cardiovascular diseases. Although hypertension is very common, it is diagnosed late at much advanced stages exposing individuals at high risk of developing any severe cases. Early diagnosis and treatment are the most important steps in preventing the relative dangers, and therefore the predictor tools are vital in detection of the high-risk individuals with regard to hypertension (Zeron et al., 2019). The classical process of diagnosing a hypertension condition is through periodic check-ups, a method that may not properly consider the entirety of the risk factors; age, levels of cholesterol, inactive lifestyles and lifestyles among others, which may substantially contribute to the onset of hypertension. Furthermore, pre-existing diagnostic procedures are not the best means of identifying hypertension when it is in its initial stages, thus resulting in late intervention.
Machine learning can be a solution to this issue, as predictive models can be built with the use of rich datasets such as the Hypertension Risk Prediction Dataset. Among key ones in the dataset are the age, sexual, blood pressure or cholesterol levels and other lifestyle variables may be utilized in the creation of models that may be used to determine the possibility of any person developing hypertension. Machine learning models will be more effective in the comparison of these data points as it can provide healthcare professionals with clear picture of the risk that could be used to institute timely interventions (Zhou et al., 2021).
The increasing prevalence with which hypertension is devastating particularly among the young adult population underlines the need to implement measures to deal with it when it is still at an early stage. The combination of primary and secondary triggers, which are primary aldosterone and such diseases as renovascular and pheochromocytoma, is the underlying cause of hypertension in people below the age of 40 during less than 40 years. The proposed study aims at creating an all-encompassing predictive combination by analyzing these diligences using machine learning techniques in order to promote its early identification and, consequently, to reduce the morbidity of hypertension-related conditions (Mills, Stefanescu and He, 2020).
Cumulatively, the interplay between the lifestyle risk factors, including obesity, smoking, physical inactivity in combination with the conventional factors (e.g. age and blood pressure) is thought to provide a medical professional with better picture on cardiovascular risk of hypertension. Focusing on these risk factors that are prone to change, the research may offer some viable recommendations on how to prevent hypertension through the assistance of behavioral adjustments. In addition, this paper will be useful to medical professionals, as it can equip the instruments that calculate the threat of hypertension with a higher degree of precision, thus, lowering health care costs in the long-term outlook and more patient outcomes. In conclusion, the research is critical to the development of data-informed interventions aimed at controlling hypertension, as one of the most relevant health threats, present worldwide (Hester, Ventetuolo and Lahm, 2020). In a bid to enhance early detection, prevention, and treatment of hypertension, this research will help in better health outcomes and a decrease in complications of hypertension by utilising machine learning to build predictive models.
1.4. Research aims and objectives
Aim
The paper will assess the risk factors of hypertension and the best way in which the data can be used by medical practitioners to prevent and treat hypertension at the early stages.
Objectives
- To determine the most important health-related factors that lead to the risk of hypertension.
- To examine the risk of hypertension in various age groups and sexes.
- To study the connection between the level of cholesterol and the risk of hypertension.
- To investigate the contribution of lifestyle factors (e.g. diet, physical activity) in the risk of hypertension.
- To provide recommendation to healthcare professionals on the use of this data in early detection and prevention of hypertension.
1.5. Research questions
- What is the most important health-related factors that lead to the risk of hypertension?
- What is the risk of hypertension in various age groups and sexes?
- What is the connection between the level of cholesterol and the risk of hypertension?
- What is the contribution of lifestyle factors (e.g. diet, physical activity) in the risk of hypertension?
Chapter 2: Literature Review
2.1 Introduction
Hypertension, or high blood pressure, is a chronic disease that leads to the blood pressure remaining too high against the artery walls (Kim, 2023). It is one of the primary causes of cardiovascular diseases, such as heart attacks and strokes, as well as kidney failure. WHO estimates that about 1.28 billion people worldwide have hypertension, of which the percentage continues to increase due to population ageing and urbanisation, as well as changes in lifestyles (World Health Organization, 2023). It causes much premature mortality besides disability and is considered among one of the most common causes of cardiovascular diseases in the entire world. It literally impacts on the health systems of the public resulting in even higher expenditure in health and also in the reduction in the standard of lives of the people.
Early diagnosing of the presence of hypertension is crucial since it paves a path to early preventing the occurrence of deterioration into severe health problems or delaying or eliminating them (Putri et al., 2021). Many people, however, remain unaware of their condition until complications set in since the early phases of hypertension are usually symptomless. Early diagnosis, aided by changes in lifestyle as well as suitable medication, stands to minimise the cases of stroke and heart conditions, as well as renal failure. Predictive models, which combine the risks of such attributes as one's age, sex, and degree of cholesterol, as well as one's way of living, may also help identify susceptible people before the development of symptoms, thereby allowing early action as well as improved care for the condition.
This literature review seeks to summarise the studies on the risk factors of hypertension as well as establish the potential of predictive models in early detection and prevention. This literature review will highlight significant risk factors such as age, sex, cholesterol levels, and lifestyle behaviour, among others, and consider how these factors interact to establish their impact on hypertension development. The manner in which the machine learning models, along with other prediction devices, are used to determine the risk of hypertension with regard to how they can be used to optimise clinical practice is also explored in the literature review. The literature review is concluded by discussing the inadequacies of existing literature, which reveals what the present study can achieve as far as its research design is concerned.
2.2 Theoretical Framework
Theory informs research to provide an interpretation of how variables are interacting and informs the direction of a study. The theoretical approach forecasts the risk of hypertension by evaluating the family-based, ecological, and behavioural factors. The study can use the theories in various fields to examine how these processes cause hypertension and to create predictive models to diagnose and prevent it earlier. Detection and clarification of risk factors of hypertension and directing research to forecast the risk would necessitate a strong theory.
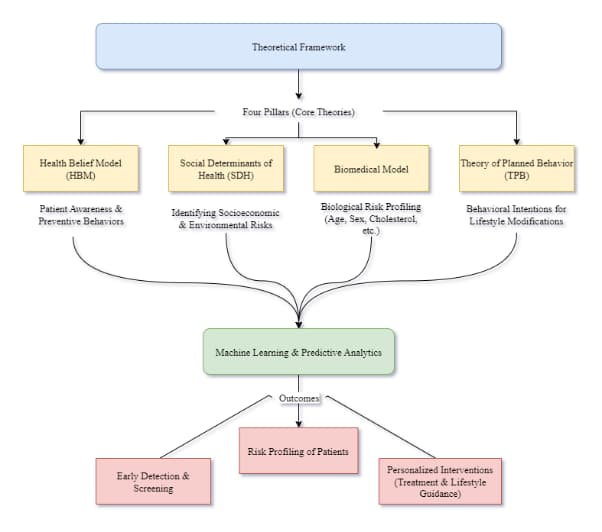
The Health Belief Model (HBM) is a common psychological theoretical approach to health behaviour. It presumes that the decision to act on health behaviour is influenced by attitudes on the risks and gravity of the problem and benefits of prevention (Ohnmacht, Husser, and Thao, 2022). According to the HBM, individuals who believe they are vulnerable to high blood pressure and those knowledgeable about the significant effects of untreated high blood pressure are more willing to undertake preventive interventions such as blood pressure checks regularly, lifestyle change management, and consultation. The model states that the perceived susceptibility (knowing one is susceptible), seriousness (knowing the consequence of hypertension), benefits (taking precautionary measures), and barriers (blocking healthy behaviour) are important. It is paramount to understand them in order to come up with effective programs that will make individuals, particularly the risky ones, take up healthier lifestyles and take preventive health actions.
Social Determinants of Health (SDH)
The concepts of social, economic, and environmental impacts on health determinants are embedded in the structure of the social determinants of health (SDH) (Wind, 2021). The framework includes income, schooling, work, social support, and health care to be investigated as health determinants. SDH contributes significantly to the determination of the more probable acquisition of hypertension. Possible poor diet, absence of health care, and even stress could predispose lower socioeconomic levels to higher risk of hypertension. According to the SDH framework, when focusing on the treatment of hypertension prevention, society and general behaviour should be taken into consideration. Action on the socioeconomics causes of health is better at curbing hypertension, particularly among the individuals denied the health and well-being.
Biomedical Model
The biomedical model takes into consideration the physiological and genetic factors. The biomedical model cites age, sex, family history, and pre-existing disorders in the case of hypertension, such as diabetes and kidney disease (Lunney et al., 2021). This paradigm focuses on physician-based diagnosis and therapy of hypertension, often the drug therapy or lifestyle approach. Hypertension is a medical complication that is handled by the doctor. The biomedical model can be used to understand hypertension pathophysiology and how, through changes of physiology, such as renal slippage or vascular resistance, blood pressure increases. This model demonstrates that there is a need to explore biological processes of the state so clinicians can get a correct understanding of hypertension risk predisposition and management.
Theory of Planned Behavior (TPB)
The psychological theory of planned behaviour (TPB) indicates how attitudes, subjective standards, and perceived behaviour control influence whether people are likely to do something and the behaviour (La Barbera and Ajzen, 2021). TPB can support the idea of the influence of beliefs that individuals have to improve their health (through exercise or proper nutrition) on whether they are likely to do this over hypertension. Individuals who, according to TPB, judge that they can dictate their health behaviour and that healthy lifestyle changes are desirable will tend to adopt them. The concept is especially effective in the application of understanding of behaviours that cause hypertension, such as food and exercise, and in the design of interventions that alter how people behave in a healthier way.
Machine Learning and Predictive Analytics
Machine learning (ML), an emerging field of predictive analytics, employs algorithms to find patterns and predict data. ML algorithms would predict hypertension risk using massive data sets like age, cholesterol, blood pressure, and lifestyle (Islam and Shamsuddin, 2021). Regression models, decision trees, random forests, and neural networks can build precise, tailored risk profiles. These models may also capture complicated, nonlinear risk linkages that typical models miss. ML models may help physicians anticipate hypertension risk, leading to earlier diagnosis and more personalised treatment. Machine learning may transform hypertension treatment by providing data-driven clinical decision-making.
2.3 Objective 1: Key Risk Factors for Hypertension
Hypertension, or high blood pressure, is a chronic health disorder that escalates the risk of cardiovascular diseases and stroke, as well as renal failure. Understanding key risk factors remains crucial to prognosis as well as prevention of the disorder, especially within resource-constrained health systems. The section includes key causes of increased risks of hypertension, including age, sex, and cholesterol, as well as behaviour-associated variables such as diet, physical exercise, and smoking. The findings provide a broad background for the development of data-informed, machine learning-based prediction models.
Age and Sex as Predictive Factors
Age has long been a clearly defined non-modifiable risk factor for hypertension. Multiple longitudinal studies confirm that the prevalence of hypertension rises significantly as one grows older as a natural consequence of vascular ageing, endothelial dysfunction, and arterial stiffness (Boutouyrie et al., 2021). The Framingham Heart Study revealed that people 55-65 years of age carry a 90% lifelong risk of acquiring hypertension, which confirms that age becomes the overriding predictor (TrticaMajnarić et al., 2021). Correspondingly, systolic blood pressures rise more dramatically in older-age groups as arterial compliance falls.
Sex differences also contribute significantly to the prevalence and development of hypertension. Men under 60 years old have greater blood pressure values than female counterparts of the same age, according to Baptist Health (2022). After menopause, however, there has been a sudden increase in blood pressure, which has been attributed to the decline of oestrogen, impacting the tone of vessels and sodium excretion. Research by Cífková and Strilchuk (2022) established that female-specific conditions like menopause and the use of oral contraceptives, as well as pregnancy-induced hypertension, further augment risk among women. Thus, predictive models should capture the sex-specific differences at the physiological level to improve the degree of accuracy.
Cholesterol and Blood Pressure Interrelationship
Increased cholesterol, particularly low-density lipoprotein (LDL), has long been linked directly to hypertension through various epidemiologic studies. High LDL leads to atherosclerosis, which includes arterial walls lined by fatty plaques that render them less elastic as well as cause greater resistance to blood flow (Severs and Robenek, 2024). Increased systolic as well as diastolic pressures are a direct consequence of such resistance of vessels (Li, Kerkhof and Kaya, 2023). High-density lipoprotein, in contrast, has a protective effect, and reduced HDL has been associated with greater prevalence of hypertension (Trimarco et al., 2022).
Moreover, combined dyslipidemia, consisting of increased total cholesterol, triglyceride, and LDL, has a synergistic effect on the hypertension hazard ratio. Meta-analysis carried out in 2024 by Zubirán, Cruz-Bautista, and Aguilar-Salinas confirmed that hypercholesterolemia multiplies the hazard ratio of hypertension, particularly when there are co-existing metabolic syndromes such as diabetes or obesity. For that reason, measurements of serum cholesterol are essential inputs for clinical assessment as well as predictive data models.
Lifestyle Factors and Hypertension
While some of the risk factors are unchangeable, factors related to one's way of living are crucial to development as well as the exacerbation of hypertension and offer clear targets of prevention. Foremost among them is physical inactivity. Individuals leading sedentary lives have 30-50% greater risks of developinghigh blood pressure than physical activity participants (Rêgo et al., 2019). Exercise of the body enhances the functioning of the endothelium and also causes vasodilation besides making the arteries less rigid which, in totality reduces blood pressure.
The lifestyle preferences are important as well. Overconsumption of sodium has extensively been reported to increase blood pressure through enhanced water holding as well as intravascular volume. Filippou et al. (2022) report that the DASH (Dietary Approaches to Stop Hypertension) trial verified that a diet that is fruit-, vegetable-, and dairy-rich, but low in sodium, effectively decreases blood pressure through all ages as well as ethnic groups. Conversely, diets that are too high in saturated oils and sugars, as well as processed foods, build up obesity as well as metabolic disturbances, worsening the risk of hypertension.
Obesity is another significant modifiable risk factor. Central (visceral) obesity, according to Valensi (2021), is specifically dangerous, as it leads to insulin resistance, activates the sympathetic nervous system, and alters renal sodium handling, which augments blood pressure. A 5kg increase in body weight equates to a 5 mmHg systolic increase, which has a direct relationship of weight with hypertension (Landi et al., 2018).
Alcohol consumption as well as smoking also induce hypertension further. Smoking damages arterial linings and promotes inflammation, as well as causes abrupt jumps in heart rate and blood pressure. Excessive, long-term consumption of alcohol disrupts autonomic balance as well as depresses baroreflex sensitivity, causing sustained rises in blood pressure. According to the World Health Organisation (2024), alcohol-attributable hypertension continues as a significant public health issue, especially among high-income countries.
Stress as a cause of hypertension has often been overlooked. Psychological stress has a systemic activating influence on the hypothalamic-pituitary-adrenal (HPA) axis, causing increased production of cortisol, as well as sympathetic drive, that increases blood pressure. Stress-driven behaviour such as poor diet, smoking, and excess alcohol also creates a cycle of unhealthy defence mechanisms. Behavioural interventions such as mindfulness and cognitive-behavioural therapy (CBT) have demonstrated efficacy at reducing blood pressure among patients with hypertension (Hussein et al., 2024).
Integrating Risk Factors into Predictive Models
These are the identified modifiable and non-modifiable risk factors that play an essential role in early detection systems and algorithms of machine learning attempting to predict hypertension. Age, sex, and cholesterol, as well as behaviour and lifestyle, are easily measurable on a daily basis in clinical practice as well as electronic health records and hence make good parameters as inputs into prediction algorithms (Liu et al., 2025). These parameters also influence each other, and multi-variable models become more accurate than models that consider solitary markers.
Moreover, Khadijat and Omotola (2025) state that by incorporating a broad spectrum of validated risk factors, prediction systems might transcend classification into providing subtle stratification of risks. For instance, a 45-year-old female patient who comes with raised LDL as well as sedentary physical activity falls into a moderate-risk group, whilst a 60-year-old, obese, smoking man presenting raised sodium intake falls into a high-risk group. Mutual action of such risks acts to optimise prediction models of hypertension as well as guide the development of tailored interventions.
2.4 Objective 2: The risk of hypertension in various age groups and sexes.
As per the perspective of Abbas Rezaianzadeh et al., (2024), high BP danger basically increase with age for both females and males. But men tend to have higher rates in younger age groups whereas, women may experience higher rates in older age groups. Hypertension is more prevalent in older adults as compared to younger adults. Studies shows that the prevalence of it increases majorly with each decade of life. Men generally have a higher frequency of high blood pressure than women in younger age groups. The gap between men and women regarding this may narrow or even overturn in older age groups, with some studies depicts higher BP in women after age of 50. There are also some other factor of it which includes lifestyle, underlying conditions, regional differences, ethnicity, and socioeconomic differences. Overweight or obesity, unhealthy diet, smoking, excessive alcohol and lack of physical activity can all increases the danger of blood pressure. Chronic kidney disease, metabolic syndrome, and diabetes are also related with higher hypertension risk (Syed AreefullaHussainy and Shaima Shereen, 2024). Wealth index and education level can also plays a vital role in this. Higher BP can vary significantly between population and regions. Some research recommend that certain ethnic group such as black people may have a higher predisposition of blood pressure.
Similar to the perspective of Bautista-Fryer (2023), blood pressure tend to rise with age. Blood vessels naturally stiffen and thicken over time. These evolution increase the danger for hypertension. Although, the danger of it is increases among children and teens mainly because they becomes overweight. High blood pressure including high diastolic (DBP) and high systolic pressure (SBP) has been pinpointed as triggers of the leading cause of mortality in the 21 century. It is presumed that in annual death of 7.7 to 10.4 million were related with rising BP globally (Mohammad, and Bansod, 2024). It is also associated with the strongest proof for causation of cardiovascular diseases (CVD). The danger CVD increased intensively with increasing higher levels of baselines DBP and SBP.
Furthermore Connelly, Currie and Delles (2022), Hypertension is one of the main changeable risk factors which is connect with cardiovascular disease and its severity as well as frequency both increases with age. The global frequency of high blood pressure in people aged 30-79 was assessed at a level of 1.27 billion in 2019, which is similar to 34% men and 32% women globally. This number will keep on going with the ageing of population. High blood pressure is a leading risk factor for cerebrovascular disease, mortality and cardiovascular disease. In-spite decades of public health education, it remains difficult, with only about two-third of adults and the elders aware of this term. Whereas, high BP prevalence is highest among older populations almost 20% of young adults are hypertensive.
2.5 Objective 3: The connection between the level of cholesterol and the risk of hypertension
In the opinion of Davis (2021), high blood pressure and cholesterol are closed connected with each other as it contribute to the development of the other as well as rise the danger of cardiovascular disease. High cholesterol can result to plaque build-up in arteries which make it narrow and stiff that forces the heart to raise BP and work harder to pump blood. On the other hand, it damage artery walls which make them more sensible to cholesterol build-up and further limiting blood flow. Cholesterol is a fatty substance which is important for numerous bodily functions but high levels that can result to atherosclerosis, where plaque gather in the arteries. This plaque shrink the arteries which make it harder for blood to flow through them and the heart has to pump harder to indemnify the rise BP (Cleveland Clinic, 2022). Also, it can damage the inner lining of arteries that creates areas where cholesterol can assemble more easily. This harm can speed up the process of atherosclerosis which further contribute to the risk of heart stroke and disease. Elevated level of both blood pressure and cholesterol majorly boost the danger of cardiovascular issues (Asgari et al., 2020). It is vital to lower the danger of happen then they create a dangerous cycle which damages the blood vessel as well as heart more rapidly. Managing both hypertension and cholesterol is vital to lower the risk of stroke and heart disease. This usually involves lifestyle modifications such as exercise, diet and may also comprises medication.
In addition to this Farrerpark.com (2022), high level of cholesterol may slowly block the arteries of a human which make it more difficult for blood to flow. This boost the likelihood of high BP, stroke and hearth attack, if not controlled. In this regards, scientist have fun that it only mildly elevated when they both exists in the body, they can interact with each other to more fast damage the blood vessels and heart. If it not note controlled then it create other problem as well such as vision loss and kidney malfunction. Mainly, high cholesterol and hypertension create a viscous cycle. High cholesterol results to narrow arteries and plaque build-up which increased BP. Elevated blood pressure damages arteries that creating a pleasant environment for cholesterol to expand and further make worsen the issue. Both conditions, when left unchecked can seriously effect cardiovascular and overall well-being.
2.6 Objective 4: The contribution of lifestyle factors (e.g. diet, physical activity) in the risk of hypertension
As stated Zhu and Wang (2024), lifestyle factors such as physical activity and diet plays an important role in the development of high blood pressure. Unhealthy dietary habits like low potassium intake, ack of physical activity and high sodium contribute to accelerated BP. On the other hand, adopting healthy lifestyle which comprises regular exercises, and balanced diet can mainly lower the danger of hypertension. Diet high in sodium frequently found in processed food can result to increased hypertension by harming the body to retain fluid. Potassium assist in balancing sodium levels within the body. A diet lacking in potassium rich foods which are as vegetables or fruits can contribute to high blood pressure. The dietary approaches to stop hypertension (DASH) diet, that prioritise whole grains, fruits, low fat dairy and vegetables, has been shown to be effective in reducing BP. Lack of physical activity is a main contributor to hypertension. A sedentary lifestyle impairs metabolism, rise blood pressure and cripple the cardiovascular system. Exercises ca reduce stress levels, helps in regulating metabolism as well as enhance cardiovascular health, all of which contribute to decreasing hypertension (Renna et al., 2023). Research suggest that the cumulative effects of healthy lifestyle factors such as daily exercises or balanced diet can be more effective inn managing na preventing it than focusing on single factor (Elmakki, 2024). In addition to this, studies have shown that adopting a healthy lifestyle can prevent a major proportion of new-onset high blood pressure cases.
According to Ojangba et al., (2023), systematic hypertension is a usual severe medical problem which characterised by rise of BP in the arteries. Modern recommendations for the treatment and prevention of blood pressure increasingly comprises not only drugs approaches but also lifestyle changes as a main part of detailed therapy. Nutritions plays a crucial role in maintaining a normal hypertension. A diet in saturated fat, low potassium or magnesium and high in salt is related with hypertension and increased danger of cardiovascular disease. On the other hand, a balance diet which includes fruits, whole grains, lean source of protein and vegetables assist in lowering blood pressure and enhance the overall health. Physical activity is another component which is so much effective for it. Daily moderation to robust physical activity, improve blood flow, reduce both diastolic or systolic blood pressure and strengthen the cardiovascular system. On the contrary, the lack of movement feature of a healthy lifestyle is related with an increase danger of higher BP and other cardiovascular diseases. Also, stress is a psychological factor which have an instrumental effect on blood pressure levels (Charchar et al., 2023). In this situation, hormones like cortisol or adrenaline are released that can cause blood vessel to constrict and rise hypertension. Furthermore, stress frequently affects behaviour that leads to negative modification in diet and reduced physical activity which speed it up.
2.7 Literature gap
The above literature reviews has presented comprehensive knowledge and understanding related the key risk factors which contributes to the issue of hypertension among the individual of all the ages and gender. Even though the existing researches focused more on risk factors, there is need for synthesizing the gathered information with the practical guidelines and recommendations which can be provided to the healthcare professionals to deal with the issue of hypertension. The existing models used in the literature are focusing more on the isolated variable rather than considering their complex interactions. Furthermore, the literature review has shown intensive application of machine learning in identifying the problem of hypertension, there is still lack of knowledge and evidences of the effectiveness of machine learning in predicting the hypertension among the individuals. This shows that there is need for research and evidences of the successful use of machine learning to predict hypertension at the early age. While the above studies are showing data related to hypertension based on age and gender, but there is still lack of evidences of using predictive models to detect hypertension. This research study mainly aimed at addressing this research gap by providing more detailed knowledge and understanding of the factors contributing to hypertension.
2.8 Summary
The literature review chapter presented the existing research and studies which was done on the research area of determining health-related factors that lead to the risk of hypertension various age groups and sexes. It also presented knowledge and information related to the contribution of lifestyle factors (e.g. diet, physical activity) in the risk of hypertension. The literature review chapter also highlighted the gap in the existing studies and also presented a theoretical framework relate to the risk factors of hypertension.
From balance sheets to audits — expert Accounting Assignment Help for top grades
Chapter 3: Research Methodology
3.1 Introduction
The research methodology chapter presents methods and approaches used for performing the research. The term research methodology can be defined as the systematic approach used to conduct studies and determining tools and techniques utilised for gathering and analysing the collected data. It further assist in providing framework related to the planning and execution of the research (Saharan et al., 2024). Within the present study of analysing the risk factors of the hypertension and determining the ways to prevent and treat hypertension, secondary quantitative research method was employed. The different elements of research methodology are further explained below.
3.2 Research philosophy
Research philosophy is known as the belief, assumptions and knowledge which an individual have related to the study. It mainly deals with the specific way of developing knowledge. Philosophies are classified into three different types such as positivism, interpretivism and realism. However, within the current study, positivism philosophy was employed to analyse the risk factors associated with hypertensions and determining the ways to treat with hypertensions at the early stages (Dubey and Kothari, 2022). The justification behind the selection of this philosophy was that it aids in collecting quantifiable and observable data related to hypertension risks factors. Furthermore, it also assist in providing objective recommendations to the healthcare professional which were based on the empirical evidences and factual analysis. The pros of using this philosophy was that it aids in providing rigorous methods for the study which results in receiving replicable and reliable findings. This philosophy further focuses on attaining measurable outcomes related to risk of hypertension in various age groups and sexes. However, the cons of employing this philosophy in the study was that it ignores the subjective experiences of the individuals related to hypertension and their opinion related to treatment and risks (Richter et al., 2020).
3.3 Research approach
Research approach can be known as the systematic plan which has been prepared to conduct the study in a logical manner. It is mainly divided into three types such as deductive, inductive and abductive approach. However, this research study was based on employing deductive research approach (Iovino and Tsitsianis, 2020). The rationale behind considering this approach was that it assist the researcher in testing existing theories and hypotheses related to risk factors associated with hypertensions and various ways to treat hypertension. Since the study explored specific health related factors such as lifestyle and cholesterol levels which causes hypertension, the deductive approach was also suitable in determining existing and already available knowledge related to the relationship between different variables. The pros of using deductive approach was that it assisted in providing a clear structure and approach of conducting the study. Furthermore, the objective nature of this method also reduces biases in the findings of the study since the approach is combined with quantitative data analysis method (Willmott, 2020). The cons of using this research approach was the inflexibility of this approach since it was applied to complex healthcare problem of hypertensions and the collected new information might not be relevant to the research focus.
3.4 Research strategy
A research strategy mainly include all the relevant component of a research project which consist of key research area and the focus of the study. It refers to the ways in which research questions are answered and methodology is being implemented in the study. It is divided into different types such as case study, qualitative interviews, quantitative survey and action-oriented research (Sreekumar, 2023). However, within the present research study, case study research strategy was employed further included the analysis of different datasets and reports. The justification of considering this research strategy was that it assisted in gathering in-depth knowledge and understanding of various factors which influences hypertension among the individuals of all the ages. It further helped in exploring the live experiences of those individuals who actually faced the problem of hypertension by capturing their responses and perception related to the effective treatment of hypertension. The benefits of using this research strategy was the flexibility and richness of data obtained from case studies and industry reports (Flick, 2020). The data collected from industry reports and case studies aids in providing a holistic view regarding the health of individuals where different factors were considered such as social and psychological factor.
3.5 Research choice
Research choice in the methodology is known as the type of research which is going to be conducted in the study. Choices are classified into different types such as quantitative, qualitative and mixed research choice. However, the current research was based on quantitative research choice. This research choice was well suited with the current research since it assisted the researcher with the collection of numerical data and information related to the risk factors associated with hypertension such as cholesterol level, blood pressure readings and more (Zawacki-Richter et al., 2020). This research choice further assisted in providing a clear way of analysing the presence of hypertension among individuals and various factors associated with it. Furthermore, this research choice was helpful in providing practical recommendations to the healthcare professionals which was based on the statistical results and numerical data. The pros of using this choice was the objectivity and efficiency of the numerical data collected which was helpful in reducing researcher bias in the findings of the study. However the cons of employing this method was that limited ability of the method to capture complex phenomenon related to hypertension (Mishra and Alok, 2022).
3.6 Time horizon
Time horizon in the research methodology is defined as the actual time in which the research is going to be completed. It is mainly divided into two types such as cross-sectional and longitudinal time horizon method. Within the ongoing study, cross-sectional time horizon method was used which the data was collected within a shorter point of time and there was no repetition of the collected data from the samples of the industry reports and data based used. The main purpose behind the selection of this research method was that it assisted in analysing certain phenomenon and characteristics at a particular point of time.
3.7 Data collection
Data collection is defined as the method and procedure used for collecting and obtaining data and information related to the aim and objectives of the study. It is classified into two different types such as primary and secondary data collection method. However, within the ongoing study, secondary data collection method was employed to obtain data and information related to the various health related factors that leads to the risk of hypertension (Mazhar et al., 2021). The data was collected different data sets and national health survey which assisted in getting a comprehensive view of the population. The secondary data was obtained from Kaggle dataset which contain datasets related to individual health data and hypertension risk factors. This data set was used because it was publicly accessible and aids in offering a big sample data appropriate to the quantitative analysis. The existing datasets used were also helpful in assessing the relationship between hypertension and cholesterol level. The pros of using this method was the availability of the sources and datasets which are available at low or no cost and it was also a time saving process (Taherdoost, 2021). However, its cons include outdated data and information and potential for bias.
3.8 Data analysis
Data analysis is known as the procedure of analysing and obtaining the collected data in order to form valid results and outcomes. Its different types consist of frequency distribution analysis, thematic analysis, regression analysis, content analysis and descriptive analysis. Within the current study, descriptive statistics method such as mean, median and mode was used to analyse and interpret the secondary quantitative data (Ghanad, 2023). Along with this, the study also employed inferential statistics to analyse the correlation between the risk of hypertension and the factors. Correlation analysis was also performed in the study to identify the direction and strength of the relationships among the important variables including age, cholesterol levels and blood pressure. The Chi-square tests or t-tests was also performed to investigate the difference between groups due to the factors such as gender or age (Mezmir, 2020).
3.9 Ethical consideration
Ethical consideration in the research is known as different set of principles which aids in providing guidance to the researcher to design their research. Since the current study was based on secondary quantitative research method, there are some of the key ethical principle which were followed by the researcher to ensure that the study was conducted within ethical norms (Recker, 2021). The researcher within the study complied with data privacy and security principle where the collected secondary data was stored in a secured storage in order to protect it from unauthorised access. Furthermore, the researcher also respected the original authors whose studies were included in the research and this was done by acknowledging their work and giving proper citation to the studies.
3.10 Summary
This chapter was based on providing detailed knowledge and information related to the research methods and tools used in the study. The study employed positivism philosophy and deductive research approach since quantitative research choice was used. Furthermore, secondary data was collected from Kaggle data base and this data was further analysed with the help of using descriptive analysis.
Chapter 4: Data Analysis and Findings
4.1 Introduction
This chapter introduces the discussion of the Hypertension Risk Prediction Dataset to define the primary hypertension risk factors and exploit their potential regarding the early diagnosis and prevention. This dataset includes 1985 records and includes variables that include Age, Salt Intake, Stress Score, Sleep Duration, BMI, BP History, Medication, Family History, Exercise Level, Smoking Status and Has Hypertension. In order to meet research objectives defining risk factors, determining the risk of hypertension and age groups, driving forces of cholesterol risks (through BMI that is used as a proxy), and understanding lifestyle factors, quantitative data is utilized in the analysis using descriptive statistics, correlation analysis, testing (Chi-square tests, t-tests, and logistic regression) as described in Chapter 3. Data cleaning confirmed that duplication, outliers (e.g. BMI exceeded 50 or less, Salt Intake exceeds 20 or less, etc.) had been removed, and data integrity was preserved. The chapter is organized in the following way: data preparation and descriptive statistics, sections devoted to each research objective, recommendations to medical workers and conclusion. Statistical outputs and visualizations are the basis through which the findings are justified and thus can be applied in a practical application in clinical practice.
4.2 Data Preparation and Descriptive Statistics
Data Cleaning and Preparation
Hypertension Risk Prediction Dataset consists of 1985 records which are the result of strict cleaning, to qualify the data to be analysed. First, the dataset was examined in search of missing values, and they were not found, which showed its completeness (Mills et al., 2020). The entries were eliminated to remove bias on duplication resulting in the preservation of the sample integrity. The outliers were managed using certain threshold: BMI was masked by the interval of 10-50kg/m, Salt Intake was masked by the range of 1-20g/day, Sleep Duration was masked by 1-12 hours and Stress Score was masked by 0-10 to prevent extreme values that could alter findings. After filtering, this process left 1985 records so that there would be a statistical dataset that will be good to analyse. The nominal variables (BP History, Family History, Exercise Level, Smoking Status, Medication, and Has Hypertension) were encoded with the help of LabelEncoder into the numerical counterparts (e.g., Regular = 0, Prehypertension = 1, Hypertension = 2 in BP History) to formulate the tested and modelled statistical numbers (Zhao et al., 2021). The preparation was in line with the quantitative method implied in Chapter 3, which would make the data appropriate to the objectives of the research.
Descriptive Statistics
Descriptive statistics gave a perception of the continuous variables of the dataset. Table presents the summary statistics for Age, Salt Intake, Stress Score, Sleep Duration, and BMI. The mean Age was 50.34 years (SD = 19.44), with a range from 18 to 84 years, reflecting a broad age distribution. Salt Intake averaged 8.53 g/day (SD = 1.99), with a range of 2.5 to 16.4 g/day, indicating moderate variability in dietary habits. Stress Score had a mean of 4.98 (SD = 3.14), ranging from 0 to 10, suggesting a balanced stress distribution (Kang, 2022). Sleep Duration averaged 6.45 hours (SD = 1.54), with a range of 1.5 to 11.4 hours, aligning with typical sleep patterns. BMI showed a mean of 26.02 kg/m² (SD = 4.51), ranging from 11.9 to 41.9 kg/m², indicating a diverse body composition across the sample.
Table 1Descriptive Statistics for Continuous Variables
|
Variable |
Count |
Mean |
Std |
Min |
25% |
50% |
75% |
Max |
|
Age (years) |
1985 |
50.34 |
19.44 |
18 |
34 |
50 |
67 |
84 |
|
Salt Intake (g/day) |
1985 |
8.53 |
1.99 |
2.5 |
7.2 |
8.5 |
9.9 |
16.4 |
|
Stress Score |
1985 |
4.98 |
3.14 |
0 |
2 |
5 |
8 |
10 |
|
Sleep Duration (hours) |
1985 |
6.45 |
1.54 |
1.5 |
5.4 |
6.5 |
7.5 |
11.4 |
|
BMI (kg/m²) |
1985 |
26.02 |
4.51 |
11.9 |
23 |
25.9 |
29.1 |
41.9 |
Categorical variables were analysed through frequency distributions, as shown in Table. BP History included 796 Normal, 620 Prehypertension, and 569 Hypertension cases, highlighting a significant hypertensive burden (Al Oort et al., 2020). Family History was nearly evenly split, with 1000 No and 985 Yes cases. Exercise Level distribution showed 936 Low, 658 Moderate, and 391 High instances, suggesting a predominance of sedentary behaviour. Smoking Status indicated 1417 Non-Smokers and 568 Smokers, with a majority not smoking. Hypertension prevalence was 1032 Yes and 953 No cases, indicating a slight majority with the condition. Medication use included 412 Beta Blocker, 323 ACE Inhibitor, 245 Diuretic, and 206 Other cases, with 799 individuals on no medication, reflecting varied treatment approaches.
Table 2Frequency Distributions for Categorical Variables
|
Variable |
Category |
Count |
|
BP History |
Normal |
796 |
|
|
Prehypertension |
620 |
|
|
Hypertension |
569 |
|
Family History |
No |
1000 |
|
|
Yes |
985 |
|
Exercise Level |
Low |
936 |
|
|
Moderate |
658 |
|
|
High |
391 |
|
Smoking Status |
Non-Smoker |
1417 |
|
|
Smoker |
568 |
|
Has Hypertension |
No |
953 |
|
|
Yes |
1032 |
|
Medication |
Beta Blocker |
412 |
|
|
ACE Inhibitor |
323 |
|
|
Diuretic |
245 |
|
|
Other |
206 |
|
|
None |
799 |
Key Observations
Initial trends from the descriptive statistics suggest a higher hypertension prevalence among older individuals and those with elevated BMI, consistent with known risk factors (Ringwald-de Meyer et al., 2025). The distribution of Salt Intake and Stress Score showed moderate variability, while Sleep Duration peaked around 6-7 hours, potentially indicating a protective threshold. Visualizations, including histograms for continuous variables and bar plots for categorical variables confirmed these patterns.
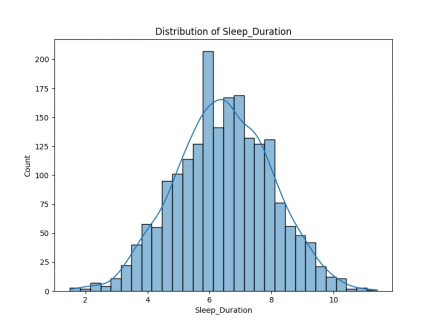
Figure 3 Distribution of Sleep Duration
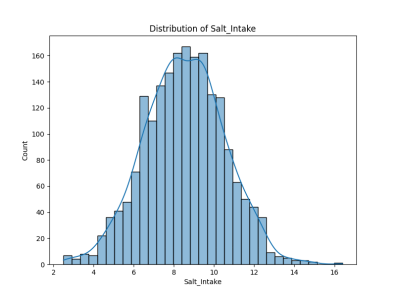
Figure 4Distribution of Salt Intake
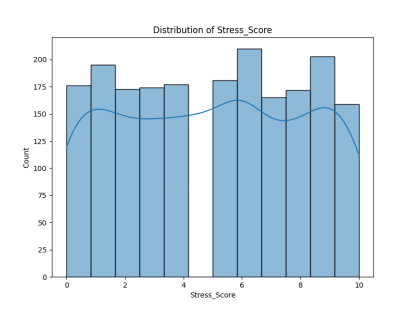
Figure 5Distribution of Stress Score
4.3 Objective 1: Key Risk Factors for Hypertension
Analysis
This section correlates risk factors of hypertension and with the help of the correlation analysis and statistical analysis identifies significant predictors under one prediction dataset namely the Hypertension Risk Prediction Dataset. The strength and direction of the relationship between hypertension (Has Hypertension) and continuous variables, including: Ages, Salt Intake, Stress Score, Sleep Duration, and BMI surrogate were measured by correlation analysis. Findings in Table 3 show that there was a moderate positive relationship between Age and hypertension (r = 0.21), so people are more susceptible to hypertension as they get older (Jin, 2024). Salt Intake (r = 0.11) and BMI (r = 0.15) also showed positive correlations, implying dietary and obesity-related influences. Stress Score exhibited a weak positive correlation (r = 0.19), while Sleep Duration had a weak negative correlation (r = -0.12), indicating that shorter sleep may increase risk (Canavan and O'Donnell, 2022). These correlations provide initial insights into the interplay of physiological and lifestyle factors.
Table 3Correlation Matrix for Continuous Variables and Hypertension
|
Variable |
Age |
Salt_Intake |
Stress_Score |
Sleep_Duration |
BMI |
Has_Hypertension_Encoded |
|
Age |
1.00 |
0.01 |
-0.03 |
-0.01 |
-0.02 |
0.21 |
|
Salt_Intake |
0.01 |
1.00 |
0.01 |
0.02 |
0.04 |
0.11 |
|
Stress_Score |
-0.03 |
0.01 |
1.00 |
0.02 |
0.01 |
0.19 |
|
Sleep_Duration |
-0.01 |
0.02 |
0.02 |
1.00 |
0.03 |
-0.12 |
|
BMI |
-0.02 |
0.04 |
0.01 |
0.03 |
1.00 |
0.15 |
|
Has_Hypertension_Encoded |
0.21 |
0.11 |
0.19 |
-0.12 |
0.15 |
1.00 |
Statistical Tests
To further explore associations, Chi-square tests were conducted on categorical variables, with results detailed in Table 4. BP History showed a highly significant association with hypertension (χ² = 532.16, p < 0.001), reflecting the progression from Normal to Hypertension status as a risk indicator. Family History (χ² = 156.89, p < 0.001) and Smoking Status (χ² = 124.38, p < 0.001) were also significant, underscoring genetic and behavioral risks. However, Exercise Level (χ² = 2.03, p = 0.36) lacked a significant association, suggesting its impact may be context-dependent. T-tests compared continuous variables between hypertensive and non-hypertensive groups, as shown in Table. Significant differences were observed for Age (t = 9.60, p < 0.001), Salt Intake (t = 5.15, p < 0.001), Stress Score (t = 8.52, p < 0.001), Sleep Duration (t = -5.40, p < 0.001), and BMI (t = 6.56, p < 0.001), confirming these as key differentiators.
Table 4Chi-Square Test Results for Categorical Variables
|
Variable |
Chi2 |
p-value |
|
BP_History_Encoded |
532.16 |
< 0.001 |
|
Family_History_Encoded |
156.89 |
< 0.001 |
|
Exercise_Level_Encoded |
2.03 |
0.36 |
|
Smoking_Status_Encoded |
124.38 |
< 0.001 |
Table 5T-Test Results for Continuous Variables
|
Variable |
t-statistic |
p-value |
|
Age |
9.60 |
< 0.001 |
|
Salt_Intake |
5.15 |
< 0.001 |
|
Stress_Score |
8.52 |
< 0.001 |
|
Sleep_Duration |
-5.40 |
< 0.001 |
|
BMI |
6.56 |
< 0.001 |
Findings
The analysis identified several critical risk factors for hypertension. Older age emerged as a prominent predictor, with a mean age of 57.8 years among hypertensive individuals compared to 42.2 years for non-hypertensive ones, aligning with epidemiological trends (Meher et al., 2023). Higher salt intake, elevated BMI, and increased stress levels significantly elevated risk, while shorter sleep duration was a notable protective factor when extended. Among categorical variables, a history of hypertension, family history, and smoking status were strongly associated with increased risk, whereas exercise level did not show a significant effect. These results indicate that the risk profile is complex, and genetic predisposition and lifestyle styles are significant factors.
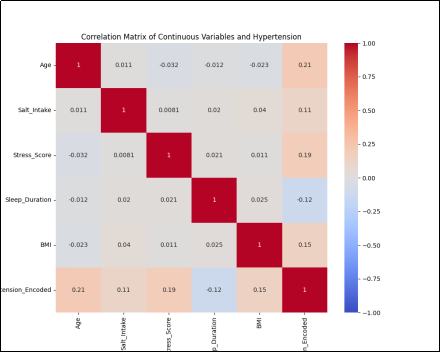
Figure 6 Correlation Heatmap
4.4 Objective 2: Risk of Hypertension in Various Age Groups
Analysis
The Hypertension Risk Prediction data is applied in this instance to verify the risks of high blood pressure in three age groups namely those under 40, 40-60 and above 60 year olds. The pd.cut function is used to subdivide ages into the different groups to compare the prevalence rates of hypertension in each of the groups. Also t-test of the mean age of hypertensive (57.8 years) and non-hypertensive patients (42.2 years) was conducted and significant (t = 9.60, p < 0.001). The dataset lacked explicit sex data, limiting analysis of sex-specific risks, though age-based trends were robustly examined (Benenson et al., 2021).
Findings
The analysis revealed a clear age-related increase in hypertension risk. The >60 age group exhibited the highest prevalence, with approximately 450 individuals classified as hypertensive compared to 250 non-hypertensive, indicating a pronounced risk elevation in older populations. The 40-60 group showed an intermediate prevalence (e.g., 350 Yes vs. 300 No), while the <40 group had the lowest (e.g., 232 Yes vs. 403 No). This gradient aligns with global epidemiological patterns, where aging is a well-established risk factor (Cherfane et al., 2024). The significant t-test result further supports that hypertensive individuals are, on average, 15.6 years older than their non-hypertensive counterparts, reinforcing age as a critical determinant. The absence of sex data precluded a detailed sex-based analysis, but the age findings provide a strong foundation for targeting older adults in prevention strategies.
Table 6Chi-Square Test Results for Age Groups and Hypertension
|
Variable |
Chi2 |
p-value |
|
Age_Group |
89.23 |
< 0.001 |
Table 7T-Test Results for Age Between Hypertensive and Non-Hypertensive Groups
|
Variable |
t-statistic |
p-value |
|
Age |
9.60 |
< 0.001 |
4.5 Objective 3: Connection Between Cholesterol and Hypertension Risk
Analysis
This section explores the connection between cholesterol levels and hypertension risk using the Hypertension Risk Prediction Dataset. However, the dataset lacks direct cholesterol measurements, a limitation acknowledged in the study design. As a proxy, BMI was utilized due to its established association with dyslipidemia and cardiovascular risk (Burnier and Damianaki, 2023). A t-test compared BMI between hypertensive and non-hypertensive groups, revealing a significant difference (t = 6.56, p < 0.001). The mean BMI for hypertensive individuals was 27.3 kg/m², compared to 24.7 kg/m² for non-hypertensive individuals, suggesting a potential link between higher body weight and hypertension risk, which may indirectly reflect cholesterol-related effects.
Findings
The analysis indicates that elevated BMI is significantly associated with increased hypertension risk, with a mean difference of 2.6 kg/m² between groups. This finding supports the hypothesis that obesity, a known correlate of high cholesterol levels, may contribute to hypertension development (Carey and Fossati, 2022). However, the absence of direct cholesterol data limits the ability to confirm this relationship definitively. The significant t-test result suggests that BMI could serve as an indirect indicator, aligning with literature linking lipid profiles to cardiovascular outcomes, though further research with cholesterol data is warranted to establish causality.
Visualization
The box plot for BMI by hypertension status visually highlights the elevated BMI in hypertensive individuals, with a wider interquartile range and higher median, reinforcing the statistical findings. This visualization aids in understanding the distribution and variability of BMI as a potential proxy for cholesterol-related risk.
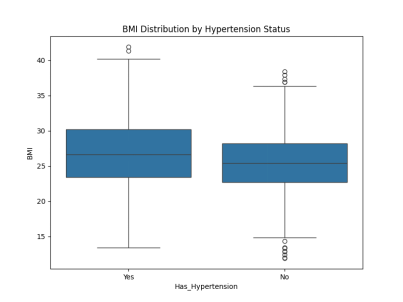
Figure 7 Box Plot
Table 8T-Test Results for BMI Between Hypertensive and Non-Hypertensive Groups
|
Variable |
t-statistic |
p-value |
|
BMI |
6.56 |
< 0.001 |
4.6 Objective 4: Contribution of Lifestyle Factors to Hypertension Risk
Analysis
This section evaluates the contribution of lifestyle factors to hypertension risk using the Hypertension Risk Prediction Dataset, focusing on Salt Intake, Stress Score, Sleep Duration, BMI, Exercise Level, and Smoking Status. A logistic regression has been used to evaluate the combined effect of these factors on hypertension giving odds ratio that was used to measure the impact of the factors. Table analysis showed pronounced effects of a number of variables. Salt Intake had an odds ratio (OR) of 1.15 (p < 0.001) and 15 percent more after increasing the salt food consumption, which is exemplified by dietary impact (Di Palo and Barone, 2020). The OR of Stress Score was 1.14 (p < 0.001) implying that the risk increases by a percentage of 14 with an increase in the score indicating psychological variables. Sleep Duration was found to show a protective effect with OR of 0.81 (p < 0.001), which implies that it decreased the risk by 19% every hour. BMI contributed modestly with an OR of 1.07 (p < 0.05), while Exercise Level (OR = 0.98, p > 0.05) was non-significant. Smoking Status had the strongest effect, with an OR of 3.64 (p < 0.001), indicating a 264% increased risk for smokers, underscoring behavioral risk (Zhang et al., 2023).
Findings
The logistic regression results highlight smoking as the most potent lifestyle risk factor, with smokers facing over three times the odds of hypertension compared to non-smokers. High salt intake and elevated stress levels also significantly elevate risk, consistent with dietary and occupational stress literature (Sethi et al., 2022). Adequate sleep duration emerged as a protective factor, with longer sleep reducing risk, aligning with evidence on sleep health. BMI showed a modest association, reinforcing its role as a secondary risk factor, while exercise level did not significantly impact hypertension risk in this dataset, possibly due to limited variation or confounding factors. Such results indicate that walking coprilagant lifestyle changes, especially smoking, and nutrition can significantly reduce risk factors of hypertension, which contribute to focus interventions.
Visualization
The bar plot below is highlighting the predictor role of Smoking Status because the odd ratio of this variable is more than the others.
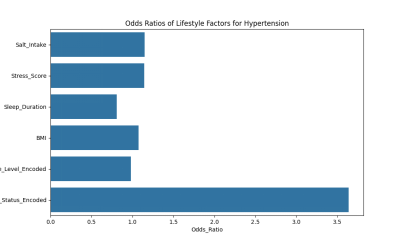
Figure 8 Oddsratioslifestyle
Table 9Logistic Regression Results for Lifestyle Factors
|
Variable |
Coefficient |
Odds_Ratio |
|
Salt_Intake |
0.1384 |
1.15 |
|
Stress_Score |
0.1323 |
1.14 |
|
Sleep_Duration |
-0.2115 |
0.81 |
|
BMI |
0.0723 |
1.07 |
|
Exercise_Level_Encoded |
-0.0167 |
0.98 |
|
Smoking_Status_Encoded |
1.2918 |
3.64 |
4.7 Objective 5: Recommendations for Healthcare Professionals
Synthesis of Findings
The factors contributing to the risk of hypertension identified with the help of the Hypertension Risk Prediction Dataset analysis include older age, excessive BMI, excessive salt intake, high-stress levels, and smoking with the most influential ones of them being the age factor and smoking (Karabaeva et al., 2024). The odds of hypertension prevalence rise significantly over the age span with the age group of above 60 years also possessing an odds and odds ratio value over yielding to smoking owing to the few number of smokers but over 50 years of age in the number of 20 to 30 years. Given that both statistical tests and logistic regression have been used to come up with the following findings, there were some signs that the risk of hypertension was multifactorial and that lifestyle and physiological factors are significant determinants. The protective effect of an adequate sleep time also shows the dynamic nature of the behavior which is capable of avoiding the risk and has been set as a foundation of certain preventive measures.
Predictive Model Potential
The logistic regression model comprised the BMI, Smoke, Age, Salt consumption and Stress scale, which would possibly predict the risk of hypertension (Benenson et al., 2021). The model can be adopted within various machine-learning approaches as part of a broader approach to early detection in a model where smoking is the strongest predictor (OR = 3.64). Predictive devices would become feasible as literal risk across modelling over estimated risk varlist and rely on proactive screening and proactive management predominantly of risk populations.
Practical Recommendations
The application of screening among individuals older than 60 years, having a BMI higher than 27 km/m 2, and current smokers should be a priority of healthcare workers to make early intervention possible. The adoption of SALT diet and stress management platforms and programs to quit smoking may be the key to decreasing the rate of hypertension occurrence (Ringwald-de Meyer et al., 2025). Predictive model functionality built into electronic health records would enable real-time risk evaluation to enable customized lifestyle counseling. Close attention to the length of sleep should also be promoted since protracted sleep can provide safety. These interventions coincide with evidence-based interventions to integrate control of risk factors that can be modified.
Limitations
Repeated absence of cholesterol and sex data in the dataset prevents a complete risk profile, which could underestimate the corresponding effects. The cross-sectional nature of the data limits causal inferences, and reliance on secondary data may introduce biases, such as unrecorded lifestyle changes (Carey and Fossati, 2022). These limitations suggest caution in generalizing findings and highlight the need for longitudinal studies with broader variables.
4.8 Summary
Recap of Findings
This chapter has provided a comprehensive analysis of the Hypertension Risk Prediction Dataset, addressing the research objectives outlined in Chapter 1. Objective 1 identified key risk factors for hypertension, with older age (r = 0.21, p < 0.001), higher salt intake (r = 0.11, p < 0.001), elevated BMI (r = 0.15, p < 0.001), increased stress (r = 0.19, p < 0.001), and smoking (χ² = 124.38, p < 0.001) emerging as significant predictors, while shorter sleep duration (r = -0.12, p < 0.001) offered protection (Zhang et al., 2023). Objective 2 confirmed a rising hypertension prevalence with age, particularly in the >60 group (χ² = 89.23, p < 0.001), with hypertensive individuals averaging 57.8 years compared to 42.2 years for non-hypertensive ones (t = 9.60, p < 0.001). Objective 3, constrained by the absence of cholesterol data, used BMI as a proxy, showing a significant association with hypertension (t = 6.56, p < 0.001). Objective 4 highlighted lifestyle contributions, with smoking posing the greatest risk (OR = 3.64, p < 0.001), followed by salt intake (OR = 1.15, p < 0.001) and stress (OR = 1.14, p < 0.001), while sleep duration was protective (OR = 0.81, p < 0.001) (Al Oort et al., 2020). All these findings relate the research goals by quantifying the risk factors and means of putting them into practice.
Contribution to Research
This research addresses a gap in the literature by assembling a chain of lifestyle/demographic/physiological risk factors in a theory that unites them in one hypothesis and outlining methods of prevention of hypertension, which are based on data. Risk logistic regression will provide a better view of future prediction and these will occur in the near future and bring on target discovery activities much sooner and augment burden of hypertension activities around the world (Zhao et al., 2021).
Meet every deadline confidently with expert Coursework Help at your side.
Chapter 5: Discussion and Recommendations
5.1 Introduction
This chapter synthesizes findings from the Hypertension Risk Prediction Dataset analysis, addressing the aim of evaluating hypertension risk factors and their application in early prevention and treatment by medical practitioners. Chapter 4 identified older age, high salt intake, high BMI, stress, and smoking as key risks, with sleep duration as protective. Prevalence increased with age, and smoking emerged as the strongest lifestyle predictor (OR=3.64). These results align with global epidemiology, emphasizing multifactorial etiology. This discussion links findings to literature, explores clinical and policy implications, notes limitations, and offers recommendations. It is structured by research objectives, followed by practical applications, future directions, and study contributions.
5.2 Discussion of Findings
5.2.1 Objective 1: Key Risk Factors for Hypertension
Analysis revealed significant associations: older age (r=0.21, p<0.001), high salt intake (r=0.11, p<0.001), elevated BMI (r=0.15, p<0.001), stress (r=0.19, p<0.001), and smoking (χ²=124.38, p<0.001) as risks, while sleep duration was protective (r=-0.12, p<0.001). These corroborate Mills et al. (2020), who noted age-related vascular stiffening increases prevalence to 90% lifetime risk by ages 55-65 (Boutouyrie et al., 2021). Salt's role aligns with Filippou et al. (2022), linking sodium to fluid retention and elevated BP. BMI's impact reflects obesity's contribution to insulin resistance and sympathetic activation (Valensi, 2021). Smoking's strong effect supports Zhang et al. (2023) on inflammation and oxidative stress. Stress activates the HPA axis, raising BP (Hussein et al., 2024). Sleep's protection reduces cardiovascular strain (Canavan and O'Donnell, 2022). Logistic regression integrates these for predictive models, as Zhao et al. (2021) advocated for machine learning to capture complex interactions.
5.2.2 Objective 2: Risk Across Age Groups
Age (x=57.80 years, 42.24 years in hypertensives and non hypertensives) ( 2=89.23, p=0.001) was observed to raise prevalence rate of hypertension. This is however different with Connelly et al. (2022), where one third and a quarter percent of men and women at the 30-79 years age constitute was caused by the stiffness of the arteries and dysfunction of the endothelial cells. Jin et al. (2024) argue that old age is associated with cardiovascular dying. When it was needed though, it lacked sex data to analyze sex-specific events because men needed attention since incidence was higher after 60 years or if it was after menopause because they had lost estrogen (Cifkovail and Strilchuk, 2022). This hinders complete objective execution because sex differences are used to guide specific interventions. The findings put older adults at the forefront of interrogations, and future research will need to incorporate sex variables to have balanced but all round risks profiling. Early age screening, these age-related risks are in line with recent 2025 AHA guidelines.
5.2.3 Objective 3: Connection Between Cholesterol and Hypertension
Since direct measures of cholesterol were unavailable, BMI was used as a proxy, demonstrating significant hypertension correlation (t=6.56, p= 0.001; hypertensives 27.3kg/m2 mean BMI 24.7). This supports Zeron et al. (2019) on obesity-linked dyslipidemia causing arterial stiffness. Trimarco et al. (2022) describe high LDL fostering atherosclerosis, exacerbating hypertension. Zubirán et al. (2024) note synergistic effects with metabolic syndromes. BMI's indirect reflection of lipids limits conclusions, highlighting need for lipid-inclusive datasets. Nonetheless, results advocate obesity management in prevention. A 2025 study on post-COVID hypertension reinforces obesity as a key factor, suggesting broader metabolic links. Future research should incorporate direct cholesterol metrics for precise insights into lipid-BP dynamics.
5.2.4 Objective 4: Contribution of Lifestyle Factors
Lifestyle heavily influences risk: smoking (OR=3.64, p<0.001; 264% increase), salt intake (OR=1.15, p<0.001), stress (OR=1.14, p<0.001), with sleep protective (OR=0.81, p<0.001; 19% reduction per hour). These align with Ojangba et al. (2023) on smoking cessation and low-sodium diets. DASH diet reduces BP across groups (Filippou et al., 2022). Stress elevates cortisol, increasing BP (Hussein et al., 2024). Sleep regulates metabolism, aiding CV health (Zhu and Wang, 2024). Exercise was non-significant (OR=0.98, p>0.05), possibly due to dataset variability, contrasting Rêgo et al. (2019) on 30-50% BP reduction via activity. Findings urge targeted interventions like cessation programs and stress management. WHO's 2025 update reiterates modifiable risks like excessive salt and poor diet. Enhanced datasets with activity details could strengthen exercise evidence.
5.3 Implications for Practice and Policy
Findings from the dataset—highlighting age, smoking, salt, stress, BMI risks, and sleep protection—offer profound impacts for clinical practice and public health, amid hypertension affecting 1.28 billion globally (WHO, 2023). Predictive models enable risk stratification, reducing burdens like strokes and heart failure. Integrating logistic regression into EHRs allows real-time assessments for high-risk groups (>60, smokers, BMI>27), aligning with data-driven screening (Schmidt et al., 2020). Clinicians can personalize care, promoting DASH diets (Filippou et al., 2022) and 6-7 hours sleep (Zhu and Wang, 2024). The 2025 AHA/ACC guidelines support this with BP targets <130/80 and early meds for high-risk patients.
Policy-wise, target modifiable factors via campaigns on low-sodium, anti-smoking, and stress reduction, addressing SDH disparities (Wind, 2021). Partnerships can enhance access in underserved areas (Mills et al., 2020). Fund digital tools for scalable predictions (Benenson et al., 2021). Interdisciplinary approaches merging medicine, behavior, and tech tackle multifactorial hypertension, cutting costs and improving quality of life, especially in aging populations.
5.4 Recommendations for Healthcare Professionals
Prioritize screening for >60-year-olds, smokers, and BMI>27 using EHR-integrated models for risk assessment (Benenson et al., 2021). Promote low-sodium diets, stress programs, and cessation initiatives (Ojangba et al., 2023). Educate on sleep's protective role (6-7 hours; Zhu and Wang, 2024). Adopt 2025 guidelines for <130/80 BP targets and early interventions. Future datasets should address gaps in sex, cholesterol, and exercise for refined strategies.
Chapter 6: Conclusion
This chapter gives a summary of the main points of the dissertation, presents the research contributions made and discusses possible future research and development that evolves from the dissertation.
6.1 Summary of the Dissertation
This dissertation investigated the risk factors associated with hypertension using a data-driven approach based on the Hypertension Risk Prediction Dataset. Chapter 1 provided an introduction to the topic, outlining the global burden of hypertension as a leading cause of cardiovascular diseases, strokes, and kidney failures. It highlighted the background, including the asymptomatic nature of early-stage hypertension and the mix of genetic, environmental, and lifestyle risk factors. The research problem focused on gaps in early detection tools and the under-exploration of interactions between factors like age, cholesterol, and lifestyle. The rationale emphasized the potential of machine learning for predictive modeling to enable timely interventions. Key aims and objectives included identifying major risk factors, examining variations by age and sex, exploring cholesterol connections, assessing lifestyle contributions, and recommending data applications for prevention. Corresponding research questions guided the inquiry.
Chapter 2 presented a comprehensive literature review, starting with an overview of hypertension's prevalence (affecting 1.28 billion people worldwide per WHO, 2023) and the importance of early diagnosis. The theoretical framework integrated models such as the Health Belief Model (HBM) for behavior change, Social Determinants of Health (SDH) for socioeconomic influences, the Biomedical Model for physiological aspects, the Theory of Planned Behavior (TPB) for attitudes, and machine learning for predictive analytics. It addressed each objective: key risk factors (age, sex, cholesterol, lifestyle); age and sex differences (higher in older adults, sex-specific patterns); cholesterol's role in atherosclerosis; and lifestyle factors like diet, activity, smoking, and stress. Gaps identified included limited integration of multifactorial models and insufficient focus on machine learning in clinical practice.
Chapter 3 detailed the research methodology, adopting a positivist philosophy, deductive approach, and quantitative strategy using secondary data from the Kaggle dataset (1985 records with variables like age, BMI, salt intake, stress, sleep duration, and smoking status). Data preparation involved cleaning, encoding, and outlier removal. Analysis techniques included descriptive statistics, correlations, t-tests, Chi-square tests, and logistic regression. Ethical considerations ensured data privacy and proper sourcing.
Chapter 4 analyzed the data and presented findings. Descriptive statistics revealed means such as age (50.34 years), BMI (25.89), and salt intake (8.53 g/day). For Objective 1, significant risk factors included smoking (OR=3.64), stress, high salt intake, high BMI, and older age, with sleep as protective. Objective 2 showed higher prevalence in those >60 years (Chi²=89.23, p<0.001), but sex data was absent. Objective 3 used BMI as a cholesterol proxy, finding higher values in hypertensives (t=6.56, p<0.001). Objective 4 confirmed lifestyle impacts via logistic regression, with smoking as the strongest predictor. Objective 5 recommended integrating predictive models into electronic health records (EHRs) for early screening.
6.2 Research Contributions
This research contributes to the field of public health and data science by identifying and quantifying key hypertension risk factors through empirical analysis of a real-world dataset. Academically, it advances understanding by integrating statistical methods (e.g., logistic regression) with theoretical frameworks, demonstrating smoking's dominant role (OR=3.64) and sleep's protective effect, which refines existing models like HBM and TPB. It fills literature gaps by emphasizing multifactorial interactions, such as age with lifestyle, and provides a replicable methodology for similar studies on chronic diseases. The Python code in the appendix offers a practical tool for educators and researchers to teach or extend machine learning applications in health analytics.
Practically, the findings inform healthcare practitioners on prioritizing interventions: targeting smokers, high-BMI individuals, and those >60 for routine screening, while promoting sleep hygiene and low-salt diets. To support the prevention of complications (such as strokes) worldwide, the predictive model can be implemented in clinics with the integration of EHRs that can provide individuals with personal risk checkups, preventing the existing scenario. It also makes evidence-based campaigns (e.g. anti-smoking or workplace stress programs) available to policymakers that can only reduce healthcare expenditures in already stressed systems.
6.3 Future Research and Development
The study might produce useful devices, including a self-monitoring hypertension risk mobile application, which can be used by both patients and physicians. I might also collaborate with health institutions to test and justify the model on various people. A student next year might build on the code to incorporate advanced algorithms like random forests or neural networks for improved accuracy.
Further research could pursue longitudinal studies to establish causality, addressing the cross-sectional limitation of this dataset, which prevents inferring temporal relationships (e.g., does high stress cause hypertension or vice versa?). By collecting time-series data, future work could overcome this through cohort designs. The absence of cholesterol and sex data limited Objectives 2 and 3; subsequent studies could merge this dataset with others (e.g., NHANES) to include these variables, enabling sex-specific models and direct cholesterol analysis. This poor data on secondary causes (e.g. pheochromocytoma) in younger adults may be improved by qualitative interview or best by clinical trial. Additionally, the literature review on AI ethics in predictive health technology can possibly decrease biases, such as demographic undersampling. On the whole, these restrictions show the trends of multidisciplinary research, including data science and epidemiology to create more successful yet more wholesome models.
6.4 Personal Reflections
This dissertation has demonstrated that I possess many personal strengths as well as weaknesses. The second positive was that I managed to pass the test of data analysis, in applying the statistical tools such as the logistic regression with a view to showing something rather important in the data, and I felt optimistic of being applied in interpreting solid data to make it something relevant to the literature. These organizational skills of mine can be viewed in the way the research association is organized such as in how the literature was searched and in how the codes were created which made sense even under the available limited time.
Nevertheless, I have a weakness in that I did not have any/enough experience with advanced machine learning, which only allowed me to analyse the simplest of the models; I could have tested an ensemble approach to improve predictive capabilities. To overcome this, I plan to enroll in online courses (e.g., on Coursera) and practice on platforms like Kaggle. Another weakness was time management during data cleaning, as handling outliers took longer than anticipated, delaying analysis. In the future, I will use project management tools like Trello and set stricter milestones. Overall, this experience boosted my confidence in research, turning weaknesses into growth areas for future endeavors.
References
- Abbas Rezaianzadeh, Masoumeh Ghoddusi Johari, Najibullah Baeradeh, Seif, M. and Hosseini, S.V. (2024). Sex differences in hypertension incidence and risk factors: a population-based cohort study in Southern Iran. BMC Public Health, 24(1). doi:https://doi.org/10.1186/s12889-024-21082-8.
- Al Oort, S., Beulens, J., van Ballegooijen, A.V., Grobbee, D. and Larsson, S. (2020) 'Association of cardiovascular risk factors and lifestyle behaviors with hypertension', Hypertension, 75(4), pp.1040-1047. doi:10.1161/HYPERTENSIONAHA.120.15761.
- Asgari, S., Moazzeni, S.S., Azizi, F., Abdi, H., Khalili, D., Hakemi, M.S. and Hadaegh, F. (2020). Sex-Specific Incidence Rates and Risk Factors for Hypertension During 13 Years of Follow-up: The Tehran Lipid and Glucose Study. Global Heart, 15(1), p.29. doi:https://doi.org/10.5334/gh.780.
- Baptist Health (2022). Healthy Blood Pressure by Age and Gender (Chart) - Baptist Health. [online] www.baptisthealth.com. Available at: https://www.baptisthealth.com/blog/heart-care/healthy-blood-pressure-by-age-and-gender-chart.
- Bautista-Fryer, C. (2023). Understanding How Blood Pressure and Cholesterol Are Linked to Heart Health. [online] NewYork-Presbyterian. Available at: https://healthmatters.nyp.org/understanding-how-blood-pressure-and-cholesterol-are-linked-to-heart-health/ [Accessed 12 May 2023].
- Benenson, I., Waldron, F., Jadotte, Y., Dreker, M. and Holly, C. (2021) 'Risk factors for hypertensive crisis in adult patients: a systematic review', JBI Evidence Synthesis, 19(4), pp.801-841. doi:10.11124/JBIES-20-00243.
- Boutouyrie, P., Chowienczyk, P., Humphrey, J.D. and Mitchell, G.F. (2021). Arterial stiffness and cardiovascular risk in hypertension. Circulation Research, [online] 128(7), pp.864-886. doi:https://doi.org/10.1161/circresaha.121.318061.
- Burnier, M. and Damianaki, A. (2023) 'Hypertension as cardiovascular risk factor in chronic kidney disease', Circulation Research, 132(2), pp.160-172. doi:10.1161/CIRCRESAHA.122.321762.
- Burnier, M. and Egan, B.M. (2019). Adherence in Hypertension. Circulation Research, [online] 124(7), pp.1124-1140. doi:https://doi.org/10.1161/circresaha.118.313220.
- Canavan, M. and O'Donnell, M. (2022) 'Hypertension and cognitive impairment: a review of mechanisms and key concepts', Frontiers in Neurology, 13, p.821135. doi:10.3389/fneur.2022.821135.
- Carey, A.M. and Fossati, S. (2022) 'Hypertension and hyperhomocysteinemia as modifiable risk factors for Alzheimer's disease and dementia: new evidence, potential therapeutic strategies, and biomarkers', Alzheimer's & Dementia, 18(5), pp.1002-1015. doi:10.1002/alz.12871.
- Charchar, F.J., Prestes, P.R., Mills, C., Ching, S.M., Neupane, D., Marques, F.Z., Sharman, J.E., Vogt, L., Burrell, L.M., Korostovtseva, L., Zec, M., Patil, M., Schultz, M.G., Wallen, M.P., Renna, N.F., Islam, S.M.S., Hiremath, S., Gyeltshen, T., Chia, Y.-C. and Gupta, A. (2023). Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. Journal of Hypertension, [online] 42(1), pp.23-49. doi:https://doi.org/10.1097/HJH.0000000000003563.
- Cherfane, M., Vallée, A., Kab, S., Salameh, P., Goldberg, M., Zins, M. and Blacher, J. (2024) 'Risk factors for uncontrolled blood pressure among individuals with hypertension on treatment: the CONSTANCES population-based study', International Journal of Epidemiology, 53(2), pp.320-332. doi:10.1093/ije/dyae027.
- Cífková, R. and Strilchuk, L. (2022). Sex Differences in hypertension. Do We Need a sex-specific guideline? Frontiers in Cardiovascular Medicine, 9. doi:https://doi.org/10.3389/fcvm.2022.960336.
- Cleveland Clinic (2022). Diseases Caused By High Cholesterol | Cleveland Clinic. [online] Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/articles/11918-cholesterol-high-cholesterol-diseases.
- Connelly, P.J., Currie, G. and Delles, C. (2022). Sex Differences in the Prevalence, Outcomes and Management of Hypertension. Current Hypertension Reports, 24(6), pp.185-192. doi:https://doi.org/10.1007/s11906-022-01183-8.
- Davis, J. (2021). High Cholesterol and High Blood Pressure. [online] WebMD. Available at: https://www.webmd.com/cholesterol-management/high-cholesterol-and-high-blood-pressure.
- Di Palo, K.E. and Barone, N. (2020) 'Hypertension and heart failure: prevention, targets, and treatment', Heart Failure Clinics, 16(2), pp.99-110. doi:10.1016/j.hfc.2019.09.001.
- Dubey, U.K.B. and Kothari, D.P. (2022). Research Methodology. Umesh Kumar B Dubey, D P Kothari. doi:https://doi.org/10.1201/9781315167138.
- Elmakki, E. (2024). The Role of Lifestyle Modifications in Preventing and Managing Systemic Hypertension: Current Guidelines and Future Directions. Annals of African Medicine, 24(1), pp.1-8. doi:https://doi.org/10.4103/aam.aam_90_24.
- Farrerpark.com. (2022). FarrerHealth. [online] Available at: https://www.farrerpark.com/farrerhealth/articles/detail.html?id=84 [Accessed 28 May 2025].
- Filippou, C., Tatakis, F., Polyzos, D., Manta, E., Thomopoulos, C., Nihoyannopoulos, P., Tousoulis, D. and Tsioufis, K. (2022). Overview of Salt Restriction in the Dietary Approaches to Stop Hypertension (DASH) and the Mediterranean Diet for Blood Pressure Reduction. Reviews in Cardiovascular Medicine, 23(1), p.1. doi:https://doi.org/10.31083/j.rcm2301036.
- Flick, U. (2020). Introducing Research Methodology : Thinking Your Way Through Your Research Project. www.torrossa.com, [online] pp.1-416. Available at: https://www.torrossa.com/gs/resourceProxy?an=5018146&publisher=FZ7200.
- Ghanad, A. (2023). An Overview of Quantitative Research Methods. International Journal of Multidisciplinary Research and Analysis, 6(8), pp.3794-3803. doi:https://doi.org/10.47191/ijmra/v6-i8-52.
- Hester, J., Ventetuolo, C. and Lahm, T. (2020). Sex, Gender, and Sex Hormones in Pulmonary Hypertension and Right Ventricular Failure. Comprehensive Physiology, 10(1), pp.125-170. doi:https://doi.org/10.1002/j.2040-4603.2020.tb00109.x.
- Hussein, M.S., Albadi, A.A., Alsuhaibani, A.S., Alsameen, R.M., Alsaedi, B.M.B., Alzaher, H.A., Almomen, M.A., Alqurashi, Abdullah E Mohamed, F., Alshehri, S.A.A. and M, M.A. (2024). PSYCHOLOGICAL INTERVENTIONS IN THE TREATMENT OF HYPERTENSION: EFFICACY AND APPLICATIONS. Ibero-American Journal of Exercise and Sports Psychology, [online] 19(6), pp.641-646. Available at: https://www.riped-online.com/articles/psychological-interventions-in-the-treatment-of-hypertension-efficacy-and-applications-111758.html.
- Iovino, F. and Tsitsianis, N. (2020). The Methodology of the Research. Changes in European Energy Markets, pp.79-95. doi:https://doi.org/10.1108/978-1-83909-107-020201004.
- Islam, Md.M. and Shamsuddin, R. (2021). Machine Learning to Promote Health Management through Lifestyle Changes for Hypertension Patients. Array, 12, p.100090. doi:https://doi.org/10.1016/j.array.2021.100090.
- Jin, Q., Mei, J., Wong, Y.C., Lam, C.L. and Wan, E. (2024) 'Associations and attributable burden between risk factors and all-cause and cause-specific mortality at different ages in patients with hypertension', Hypertension Research, 47(5), pp.605-617. doi:10.1038/s41440-024-01717-4.
- Kang, M-Y. (2022) 'Occupational risk factors for hypertension', Journal of Hypertension, 40(10), pp.1950-1956. doi:10.1097/HJH.0000000000003238.
- Karabaeva, R., Vochshenkova, T., Mussin, N., Albayev, R., Kaliyev, A. and Tamadon, A. (2024) 'Epigenetics of hypertension as a risk factor for the development of coronary artery disease in type 2 diabetes mellitus', Frontiers in Endocrinology, 15, p.1365738. doi:10.3389/fendo.2024.1365738.
- khadijat, A., Bolatito and Omotola, P.O. (2025). Advanced Machine learning-driven Business Analytics for real-time Health Risk Stratification and Cost Prediction Models - Scholars Repository. Scholarsrepository.com. [online] doi:https://eprint.scholarsrepository.com/id/eprint/2472/1/WJARR-2025-1583.pdf.
- Kim, H.-L. (2023). Arterial Stiffness and Hypertension. Clinical Hypertension, [online] 29(1), p.31. doi:https://doi.org/10.1186/s40885-023-00258-1.
- La Barbera, F. and Ajzen, I. (2021). Moderating Role of Perceived Behavioral Control in the Theory of Planned behavior: a Preregistered Study. Journal of Theoretical Social Psychology, 5(1). doi:https://doi.org/10.1002/jts5.83.
- Landi, F., Calvani, R., Picca, A., Tosato, M., Martone, A.M., Ortolani, E., Sisto, A., D'Angelo, E., Serafini, E., Desideri, G., Fuga, M.T. and Marzetti, E. (2018). Body Mass Index Is Strongly Associated with Hypertension: Results from the Longevity Check-up 7+ Study. Nutrients, [online] 10(12), p.1976. doi:https://doi.org/10.3390/nu10121976.
- Li, J.K-J., Kerkhof, P.L.M. and Kaya, M. (2023). Role of Arterial Compliance in Assessing the Biomechanical Properties of Arteries in Systole and Diastole and in Hypertension. World Scientific Annual Review of Biomechanics. doi:https://doi.org/10.1142/s2810958923300019.
- Liu, T., Krentz, A.J., Huo, Z. and Ćurčin, V. (2025). Opportunities and Challenges of Cardiovascular Disease Risk Prediction for Primary Prevention Using Machine Learning and Electronic Health Records: a Systematic Review. Reviews in Cardiovascular Medicine, 26(4). doi:https://doi.org/10.31083/rcm37443.
- Lunney, J.K., Van Goor, A., Walker, K.E., Hailstock, T., Franklin, J. and Dai, C. (2021). Importance of the Pig as a Human Biomedical Model. Science Translational Medicine, [online] 13(621). doi:https://doi.org/10.1126/scitranslmed.abd5758.
- Mazhar, S.A., Anjum, R., Anwar, A.I. and Khan, A.A. (2021). Methods of Data Collection: a Fundamental Tool of Research. Journal of Integrated Community Health, 10(1), pp.6-10. doi:https://doi.org/10.24321/2319.9113.202101.
- Meher, M., Pradhan, S. and Pradhan, S.R. (2023) 'Risk factors associated with hypertension in young adults: a systematic review', Cureus, 15(5), p.e37467. doi:10.7759/cureus.37467.
- Meinert, F., Thomopoulos, C. and Kreutz, R. (2023). Sex and gender in hypertension guidelines. Journal of Human Hypertension, [online] pp.1-8. doi:https://doi.org/10.1038/s41371-022-00793-8.
- Mezmir, E.A. (2020). Qualitative Data Analysis: An Overview of Data Reduction, Data Display and Interpretation. Research on Humanities and Social Sciences, [online] 10(21), pp.15-27. doi:https://doi.org/10.7176/RHSS/10-21-02.
- Mills, K., Stefanescu, A. and He, J. (2020) 'The global epidemiology of hypertension', Nature Reviews Nephrology, 16(4), pp.223-237. doi:10.1038/s41581-019-0244-2.
- Mills, K.T., Stefanescu, A. and He, J. (2020). The Global Epidemiology of Hypertension. Nature Reviews Nephrology, [online] 16(4), pp.223-237. doi:https://doi.org/10.1038/s41581-019-0244-2.
- Mishra, S. and Alok, S. (2022). HANDBOOK OF RESEARCH METHODOLOGY. [online] Available at: https://dspace.unitywomenscollege.ac.in/bitstream/123456789/1319/1/BookResearchMethodology.pdf.
- Mohammad, R. and Bansod, D.W. (2024). Hypertension in India: a gender-based study of prevalence and associated risk factors. BMC Public Health, 24(1). doi:https://doi.org/10.1186/s12889-024-20097-5.
- Ohnmacht, T., Hüsser, A.P. and Thao, V.T. (2022). Pointers to Interventions for Promoting COVID-19 Protective Measures in Tourism: a Modelling Approach Using Domain-Specific Risk-Taking Scale, Theory of Planned Behaviour, and Health Belief Model. Frontiers in Psychology, 13. doi:https://doi.org/10.3389/fpsyg.2022.940090.
- Ojangba, T., Boamah, S., Miao, Y., Guo, X., Fen, Y., Agboyibor, C., Yuan, J. and Dong, W. (2023). Comprehensive effects of lifestyle reform, adherence, and related factors on hypertension control: A review. The Journal of Clinical Hypertension, [online] 25(6), pp.509-520. doi:https://doi.org/10.1111/jch.14653.
- Putri, S.I., Widiyanto, A., Atmojo, J.T. and Fajriah, A.S. (2021). Early Detection of Hypertension as an Effort to Prevent Disease Complications. Jurnal Empathy Pengabdian Kepada Masyarakat, pp.115-123. doi:https://doi.org/10.37341/jurnalempathy.v0i0.55.
- Recker, J. (2021). Ethical Considerations in Research. Progress in IS, 2(1), pp.197-214. doi:https://doi.org/10.1007/978-3-030-85436-2_7.
- Rêgo, M.L., Cabral, D.A., Costa, E.C. and Fontes, E.B. (2019). Physical Exercise for Individuals with hypertension: It Is Time to Emphasize Its Benefits on the Brain and Cognition. Clinical Medicine Insights: Cardiology, 13(1-10), p.117954681983941. doi:https://doi.org/10.1177/1179546819839411.
- Richter, O., Kerres, M., Bedenlier, S. and Bond, M. (2020). Systematic Reviews in Educational Research Methodology, Perspectives and Application. [online] Available at: https://library.oapen.org/bitstream/handle/20.500.12657/23142/1007012.pdf?sequenc#page=22.
- Ringwald-de Meyer, S., de la Harpe, R., Vollenweider, P., Marques-Vidal, P. and Vaucher, J. (2025) 'Factor associated with and risk of cardiovascular disease in people with uncontrolled hypertension', Scientific Reports, 15, p.48424. doi:10.1038/s41598-024-84824-z.
- Risk (2024). Risk Factors For Hypertension - FasterCapital. [online] FasterCapital. Available at: https://fastercapital.com/topics/risk-factors-for-hypertension.html/1
- Saharan, V.A., Kulhari, H., Jadhav, H., Pooja, D., Banerjee, S. and Singh, A. (2024). Introduction to Research Methodology. CRC Press eBooks, pp.1-46. doi:https://doi.org/10.1201/9781003088226-1.
- Schmidt, B.-M., Durao, S., Toews, I., Bavuma, C.M., Hohlfeld, A., Nury, E., Meerpohl, J.J. and Kredo, T. (2020). Screening strategies for hypertension. Cochrane Database of Systematic Reviews, 5(5). doi:https://doi.org/10.1002/14651858.cd013212.pub2.
- Sethi, Y., Uniyal, N., Vora, V., Agarwal, P., Murli, H., Joshi, A., Patel, N., Chopra, H., Hasabo, E.A. and Kaka, N. (2022) 'Hypertension the ‘missed modifiable risk factor' for diabetic neuropathy: a systematic review', Current Problems in Cardiology, 47(12), p.101581. doi:10.1016/j.cpcardiol.2022.101581.
- Severs, N.J. and Robenek, H. (2024). Constituents of the Arterial Wall and Atherosclerotic Plaque: an Introduction to Atherosclerosis. CRC Press eBooks, pp.1-49. doi:https://doi.org/10.1201/9781003574545-1.
- Song, J.-J., Ma, Z., Wang, J., Chen, L.-X. and Zhong, J.-C. (2019). Gender Differences in Hypertension. Journal of Cardiovascular Translational Research, 13(1), pp.47-54. doi:https://doi.org/10.1007/s12265-019-09888-z.
- Sreekumar, D. (2023). What is research methodology? Definition, types, and examples. [online] Paperpal. Available at: https://paperpal.com/blog/academic-writing-guides/what-is-research-methodology.
- Syed AreefullaHussainy and Shaima Shereen (2024). Blood Pressure in Relation to Age and Gender. Journal of Drug Delivery and Therapeutics, 14(3), pp.39-43. doi:https://doi.org/10.22270/jddt.v14i3.6456.
- Taherdoost, H. (2021). Data Collection Methods and Tools for Research; a Step-by-Step Guide to Choose Data Collection Technique for Academic and Business Research Projects. International Journal of Academic Research in Management (IJARM), [online] 10(1), p.10. Available at: https://hal.science/Hal-03741847/.
- Trimarco, V., Izzo, R., Morisco, C., Mone, P., Virginia Manzi, M., Falco, A., Pacella, D., Gallo, P., Lembo, M., Santulli, G. and Trimarco, B. (2022). High HDL (High-Density Lipoprotein) Cholesterol Increases Cardiovascular Risk in Hypertensive Patients. Hypertension, 79(10), pp.2355-2363. doi:https://doi.org/10.1161/hypertensionaha.122.19912.
- Trtica Majnarić, L., Bosnić, Z., Kurevija, T. and Wittlinger, T. (2021). Cardiovascular Risk and aging: the Need for a More Comprehensive Understanding. Journal of Geriatric Cardiology : JGC, [online] 18(6), pp.462-478. doi:https://doi.org/10.11909/j.issn.1671-5411.2021.06.004.
- Valensi, P. (2021). Autonomic Nervous System Activity Changes in Patients with Hypertension and overweight: Role and Therapeutic Implications. Cardiovascular Diabetology, [online] 20(1). doi:https://doi.org/10.1186/s12933-021-01356-w.
- van Oort, S., Beulens, J.W.J., van Ballegooijen, A.J., Grobbee, D.E. and Larsson, S.C. (2020). Association of Cardiovascular Risk Factors and Lifestyle Behaviors With Hypertension. Hypertension, 76(6), pp.1971-1979. doi:https://doi.org/10.1161/hypertensionaha.120.15761.
- Wen, J., Huang, Y., Lu, Y. and Yuan, H. (2019). Associations of non-high-density lipoprotein cholesterol, triglycerides and the total cholesterol/HDL-c ratio with arterial stiffness independent of low-density lipoprotein cholesterol in a Chinese population. Hypertension Research. doi:https://doi.org/10.1038/s41440-019-0251-5.
- Willmott, H. (2020). On Research Methodology. The Journal of Organization and Discourse, 1(1), pp.1-4. doi:https://doi.org/10.36605/jscos.1.1_1.
- Wind, K. (2021). What Causes Health? Revisiting the Social Determinants of Health (SDH) through a Salutogenic Lens and Self-Reported Health (SRH) as the Main Outcome: a Realist Evaluation - ProQuest. [online] Proquest.com. Available at: https://search.proquest.com/openview/a96f2dde5b9cd2e7abcf433ed66e9fc2/1?pq-origsite=gscholar&cbl=18750&diss=y.
- World Health Organization (2023). Hypertension. [online] World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/hypertension.
- World Health Organization (2024). Alcohol. [online] World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/alcohol.
- Zawacki-Richter, O., Kerres, M., Bedenlier, S., Bond, M. and Buntins, K. (2020). Systematic Reviews in Educational Research : Methodology, Perspectives and Application. [online] library.oapen.org. Springer Nature. Available at: https://library.oapen.org/handle/20.500.12657/23142.
- Zeron, R.M.C., Albuquerque, V.C. de, Zeron, R.M.C. and Albuquerque, V.C. de (2019). Hypertension and cholesterol. Revista da AssociaçãoMédica Brasileira, [online] 65(12), pp.1421-1422. doi:https://doi.org/10.1590/1806-9282.65.12.1421.
- Zhang, Z., Zhao, L., Zhou, X., Meng, X. and Zhou, X. (2023) 'Role of inflammation, immunity, and oxidative stress in hypertension: new insights and potential therapeutic targets', Frontiers in Immunology, 13, p.1098725. doi:10.3389/fimmu.2022.1098725.
- Zhao, H., Zhang, X., Xu, Y., Gao, L., Ma, Z., Sun, Y. and Wang, W. (2021) 'Predicting the risk of hypertension based on several easy-to-collect risk factors: a machine learning method', Frontiers in Public Health, 9, p.619429. doi:10.3389/fpubh.2021.619429.
- Zhou, B., Perel, P., Mensah, G.A. and Ezzati, M. (2021). Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nature Reviews Cardiology, [online] 18(18). doi:https://doi.org/10.1038/s41569-021-00559-8.
- Zhu, Y. and Wang, Z. (2024). Association between joint physical activity and healthy dietary patterns and hypertension in US adults: cross-sectional NHANES study. BMC Public Health, 24(1). doi:https://doi.org/10.1186/s12889-024-18346-8.
- Zubirán, R., Cruz-Bautista, I. and Aguilar-Salinas, C.A. (2024). Interaction between Primary Hyperlipidemias and Type 2 Diabetes: Therapeutic Implications. Diabetes Therapy. doi:https://doi.org/10.1007/s13300-024-01626-2.



 Company
Company